Likelihood of Getting Cancer Again After Thyroid Cancer
- Example written report
- Open Access
- Published:
Papillary thyroid cancer recurrence 43 Years post-obit Total Thyroidectomy and radioactive iodine ablation: a case written report
Thyroid Research volume 10, Article number:8 (2017) Cite this article
Abstract
Groundwork
Recurrent papillary thyroid carcinoma (PTC) across the offset two decades of definitive treatment (i.e. full thyroidectomy and radioactive iodine ablation) is a rare occurrence.
Instance presentation
We present a case of a 71-year old Caucasian female with a afar history of PTC treated with total thyroidectomy and radioactive iodine ablation who experienced recurrence of her affliction 43 years following initial diagnosis and definitive treatment. She presented with palpable left-sided neck mass and afterward underwent a level 2, III, neck dissection and adjuvant iodine ablation. This instance presents the latest recurrence in papillary thyroid cancer documented to date in the literature.
Decision
This case exemplifies the need for the caput and cervix surgeon, radiations oncologist, general practitioner and radiologist to consider new lateral neck mass as tardily-presenting recurrence of PTC until proven otherwise regardless of depression recurrence rates across two decades from treatment and depression prognostic run a risk scores.
Background
Papillary thyroid carcinoma (PTC) is the nigh common histological type of thyroid-originating malignancy comprising 80% of all thyroid carcinomas [i, ii]. PTC is an unencapsulated tumor with papillary and follicular structures characterized histologically by overlapping cell nuclei with footing glass appearance and invaginations of cytoplasm into the nuclei [three]. Information technology differs from the follicular variant in the absence of nuclear changes in the latter. These tumors are indolent and take a good prognosis, but frequently metastasize to regional lymph nodes in 5.iv% to thirteen% of patients afterward initial surgery [ane]. As a whole, thyroid cancer more often than not has a good prognosis with a 5-twelvemonth survival rate of 98% [4, 5]. The cornerstone of handling for PTC patients is full thyroidectomy with post-operative radioactive iodine adjuvant therapy [4, 6]. Recurrence of PTC may exist loco-regional or afar, with the central compartment typically existence the offset region to develop metastatic disease, followed by ipsilateral lateral neck nodes [7].
In a study spanning six decades (1940-1999) of PTC treated at the Mayo Clinic, recurrence rates followed a logarithmic trend, meaning that the incremental hazard of recurrence decreased in each subsequent year [two]. The tumour recurrence rates were 8% at 5 years and xi% at 10 years for the subgroup of 2305 who had localized illness that was completely excised at the initial surgery. By 25 years, the cumulative recurrence rate reached 11% and increased to 13% at 40 mail service-operative years [2]. More than 80% of recurrences took place during the first decade.
Though well-nigh recurrences occur within the first 10 post-operative years, there have been reports of loco-regional recurrences a decade or more after this initial window. Cirocchi reports that local relapses can occur as tardily as twenty years after the initial diagnosis and treatment [7, eight]. In another written report by Schlumberger et al., the authors report a recurrence of differentiated thyroid carcinoma 33 years after initial handling [nine]. In a study of 269 patients which was designed to determine the length of follow-up needed for post-op thyroid patients, the authors found that the latest recurrences happened betwixt 30 and 39 years [10]. The electric current report presents the case of a loco-regional (lateral neck) recurrence of PTC 43 years after initial treatment. To the authors' knowledge, this represents the latest PTC recurrence reported in the literature.
Case presentation
A 71 year old Caucasian female with a remote history of PTC presented with a 2-month history of palpable left-sided cervix mass. Concrete exam revealed a non-tender mass in the left lateral cervix. There were no other abnormalities identified in a full head and neck examination. There was no palpable mass in the thyroid bed. Ultrasonography of the cervix revealed an absence of normal thyroid tissue, consistent with patient's history of distant thyroidectomy, and a solid mass in the left side of the neck superolateral to the expected location of the thyroid, in level 3. This inhomogeneous mass appeared vascular and measured 2.8 cm in length by 1.vii cm in diameter. It was not felt to resemble a normal lymph node in ultrasonographic features. Nonetheless, from its appearance and anatomical location, this new mass was initially suspected to represent a lymph node or a carotid body tumour.
Computed Tomography (CT) ruled out non-nodal neck pathology, and identified the mass every bit being consistent with an enlarged lymph node (Figs. 1, 2). Over again, this study revealed no evidence of recurrence in the thyroid bed, nor other evidence of neoplastic illness.

Computed tomography (transverse plane) revealing ii.8 × ane.7 cm mass in patient'southward left lateral neck
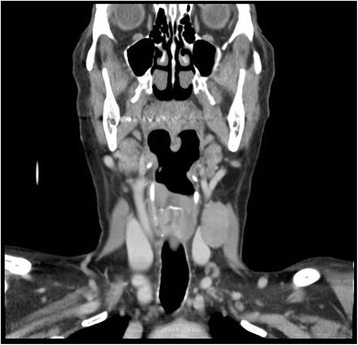
Computed tomography (coronal plane) of the patient's left lateral cervix mass
Ii fine needle aspiration biopsies (FNAs) were performed. The specimens were cellular and consisted of groups of epithelial cells in flat sheets and papillary-like clusters. The cells showed enlarged nuclei with nuclear grooves and a few intranuclear inclusions. Immunohistochemistry on the cell block was positive for TTF-ane (thyroid transcription factor ane), consistent with cells of thyroid origin.
A positron emission tomography (PET) written report was performed to dominion out distant metastatic disease. Apart from the known mass in the left neck, the PET study showed no other Fluorodeoxyglucose (FDG) avid lesions (Fig. iii). Given these diagnostic findings, the patient was scheduled for a left lateral neck dissection after obtaining informed consent. The patient after underwent an uncomplicated left level Ii-III cervix dissection under general anesthesia. A timeline of events is presented in Table 1.
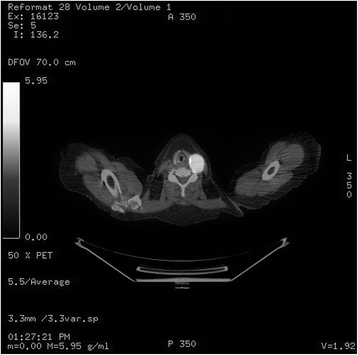
Combined CT/PET capture of fluorodeoxyglucose (FDG) uptake in left lateral neck mass
Ii of the 10 nodes sent for surgical pathology in the lymphadenectomy specimen returned positive for metastatic papillary thyroid carcinoma of tall prison cell variant. The larger of the 2 nodes measured 3.5 cm with focal extranodal extension.
The patient recovered well from the functioning and was seen for follow-upwardly three weeks following the left cervix autopsy. Given the findings from surgical pathology, it was decided that the patient would do good from radioactive iodine ablation and the patient was referred for adjuvant therapy.
Discussion and conclusions
This patient had a afar history of well-differentiated papillary thyroid cancer, which was diagnosed and treated at the historic period of 28. Her treatment consisted of a full thyroidectomy with post-operative radioactive iodine ablation therapy. Several scores have been developed to stratify patients' risk of recurrence. These scores broadly take into account patient factors, neoplasm characteristics, and the selected initial therapy. This patient would have been considered low risk for recurrence by multiple scoring systems: the European Organization for Research and Treatment of Cancer (EORTC) described by Bryar et al. [11]; The Age, Course, Extent and Size (AGES) score developed by Hay [12]; Age, Metastasis, Extent and Size (AMES) score as described by Cady and Rossi [viii]; and the distant Metastasis, patient Age, Abyss of resection, local Invasion, and tumour Size (MACIS) score [13]. More than contempo findings of associations with mutations in the BRAFV600E gene may in the future serve as a better prognosticator of distant PTC recurrence [fourteen,15,16].
A handful of studies spanning several decades post-obit postoperative thyroid cancer patients demonstrate that the majority of recurrences occur inside the first decade, and that in that location is a precipitous drop in the incremental recurrence charge per unit in each subsequent decade. These studies and a few case reports, however, do highlight that recurrence as late equally 39 years can occur. The case presented in this study details a recurrence 43 years post-obit treatment.
The extent of postoperative follow-up for patients having received thyroidectomy is informed by the relatively low rates of recurrence beyond the initial decade and the surveillance price of decades-long follow-up. The need to extend surveillance to these subsequently years is not addressed in this report and the do good of doing and then is the subject field of further report. All the same, the findings from this case serve to inform the head and cervix surgeon that recurrence has now been demonstrated to occur into the 5th decade following therapy. The authors recommend that PTC recurrence be considered high on the differential diagnosis for a new neck mass, regardless of the elapsed time following initial handling, until proven otherwise.
Abbreviations
- AGES:
-
Historic period, Grade, Extent and Size
- AMES:
-
Historic period, Metastasis, Extent and Size
- CT:
-
Computed Tomography
- EORTC:
-
European System for Research and Treatment of Cancer
- FDG:
-
Fluorodeoxyglucose
- FNA:
-
Fine Needle Aspiration
- MACIS:
-
Metastasis, patient Age, Abyss of resection, local Invasion, and neoplasm Size
- PET:
-
Positron Emission Tomography
- PTC:
-
Papillary Thyroid Carcinoma
- TTF-ane:
-
Thyroid Transcription Gene 1
References
-
Roh JL, Park JY, Rha KS, Park CII. Central neck dissection necessary for the treatment of lateral cervical nodal recurrence of papillary thyroid carcinoma? Head & neck. 2007;29(ten):901–6.
-
Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. Earth J Surg. 2002;26(8):879–85.
-
Schlumberger MJ. Papillary and follicular thyroid carcinoma. N Engl J Med. 1998;338(five):297–306.
-
Sherma SI. Thyroid carcinoma. Lancet. 2003;361(9356):501–11.
-
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(ane):9–29.
-
Hay ID, Grant CS, Bergstralh EJ, Thompson GB, Van Heerden JA, Goellner JR. Unilateral total lobectomy: is it sufficient surgical treatment for patients with AMES low-risk papillary thyroid carcinoma? Surgery. 1998;124(6):958–66.
-
Cirocchi R, Trastulli S, Sanguinetti A, Cattorini 50, Covarelli P, Giannotti D, et al. Recurrent differentiated thyroid cancer: to cut or burn. World J Surg Oncol. 2011;9:89.
-
Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery. 1988;104(half-dozen):947–53.
-
Schlumberger G, De Vathaire F, Travagli J, Vassal M, Lemerle J, Parmentier C, et al. Differentiated thyroid carcinoma in childhood: long term follow-up of 72 patients. The Journal of Clinical Endocrinology & Metabolism. 1987;65(half dozen):1088–94.
-
Grogan RH, Kaplan SP, Cao H, Weiss RE, DeGroot LJ, Simon CA, et al. A written report of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery. 2013;154(6):1436–47.
-
Byar DP, Green SB, Dor P, Williams ED, Colon J, van Gilse HA, et al. A prognostic index for thyroid carcinoma. A study of the EORTC thyroid cancer cooperative group. European Journal of Cancer (1965). 1979;15(8):1033–41.
-
Hay I. Papillary thyroid carcinoma. Endocrinol Metab Clin Northward Am. 1990;19(3):545–76.
-
Jukkola A, Bloigu R, Ebeling T, Salmela P, Blanco G. Prognostic factors in differentiated thyroid carcinomas and their implications for current staging classifications. Endocr Relat Cancer. 2004;11(three):571–ix.
-
Xing M, Westra WH, Tufano RP, Cohen Y, Rosenbaum Eastward, Rhoden KJ, et al. BRAF mutation predicts a poorer clinical prognosis for papillary thyroid cancer. The Journal of Clinical Endocrinology & Metabolism. 2005;90(12):6373–9.
-
Kim TY, Kim WB, Rhee YS, Song JY, Kim JM, Gong K, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol. 2006;65(3):364–8.
-
O'Neill CJ, Bullock M, Chou A, Sidhu SB, Delbridge LW, Robinson BG, et al. BRAF V600E mutation is associated with an increased risk of nodal recurrence requiring reoperative surgery in patients with papillary thyroid cancer. Surgery. 2010;148(6):1139–46.
Acknowledgements
Non applicative.
Funding
Not applicable.
Availability of information and materials
Data sharing is not applicable to this article every bit no datasets were generated or analysed during the current study.
Author's contributions
Authors YAT, EG, MB, MR, JT, MT, and RH have each contributed to, read, and approved this manuscript. RH and EG were directly involved in the intendance of this patient.
Author information
Affiliations
Respective author
Ethics declarations
Ethics approval and consent to participate
The demand for ethics approving was waived past the Nova Scotia Health Potency Research Ethics Board.
Consent for publication
The patient has provided their consent for the contents of this report to exist published.
Competing interests
The authors declare that they have no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open up Access This article is distributed nether the terms of the Artistic Eatables Attribution 4.0 International License (http://creativecommons.org/licenses/past/4.0/), which permits unrestricted utilise, distribution, and reproduction in any medium, provided you lot give advisable credit to the original author(southward) and the source, provide a link to the Creative Commons license, and signal if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zilch/ane.0/) applies to the information made bachelor in this article, unless otherwise stated.
Reprints and Permissions
About this article
Cite this article
Amoako-Tuffour, Y., Graham, Yard.Due east., Bullock, K. et al. Papillary thyroid cancer recurrence 43 Years following Total Thyroidectomy and radioactive iodine ablation: a case report. Thyroid Res 10, viii (2017). https://doi.org/ten.1186/s13044-017-0043-4
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s13044-017-0043-4
Keywords
- Papillary thyroid cancer
- Thyroidectomy
- Radioiodine ablation
- Recurrence
- Neck dissection
- Case report
Source: https://thyroidresearchjournal.biomedcentral.com/articles/10.1186/s13044-017-0043-4
0 Response to "Likelihood of Getting Cancer Again After Thyroid Cancer"
Post a Comment